Hay Fever, Allergic rhinitis
Published: 18 Jun 2025
ICD9: 477.9 ICD10: J30.9 ICD11: CA08.00
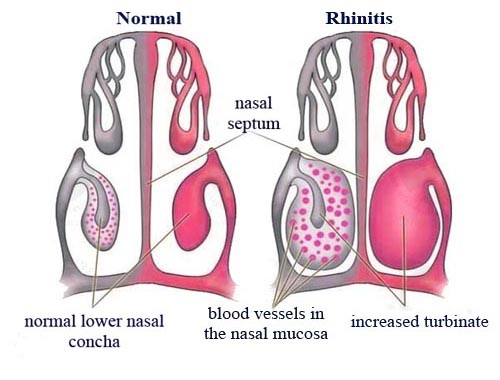
Hay fever, also known as allergic rhinitis, is an allergic reaction that causes inflammation and irritation of the nose.
It's triggered by allergens, typically pollen (from trees, grasses, or weeds), but can also be caused by other airborne particles like mold spores, dust mites, or animal dander.
Here's a breakdown of what you need to know about hay fever:
Key Characteristics:
![]() Allergic Reaction: It's an overreaction of your immune system to harmless substances (allergens). Your body releases histamine and other chemicals in response to these allergens.
Allergic Reaction: It's an overreaction of your immune system to harmless substances (allergens). Your body releases histamine and other chemicals in response to these allergens.
![]() Inflammation: This release of chemicals leads to inflammation of the nasal passages, sinuses, and sometimes the eyes.
Inflammation: This release of chemicals leads to inflammation of the nasal passages, sinuses, and sometimes the eyes.
![]() Seasonal or Perennial: Hay fever can be:
Seasonal or Perennial: Hay fever can be:![]()

![]() Seasonal: Most commonly associated with pollen during specific seasons (e.g., spring for tree pollen, summer for grass pollen, fall for weed pollen).
Seasonal: Most commonly associated with pollen during specific seasons (e.g., spring for tree pollen, summer for grass pollen, fall for weed pollen).![]()

![]() Perennial: Occurs year-round, often triggered by indoor allergens like dust mites, pet dander, or mold.
Perennial: Occurs year-round, often triggered by indoor allergens like dust mites, pet dander, or mold.
Common Symptoms:
![]() Sneezing: Frequent and often forceful sneezing.
Sneezing: Frequent and often forceful sneezing.
![]() Runny Nose: Clear, watery nasal discharge.
Runny Nose: Clear, watery nasal discharge.
![]() Nasal Congestion: A stuffy or blocked nose.
Nasal Congestion: A stuffy or blocked nose.
![]() Itchy Nose, Throat, and Eyes: An irritating itching sensation.
Itchy Nose, Throat, and Eyes: An irritating itching sensation.
![]() Watery Eyes: Red, itchy, and teary eyes (allergic conjunctivitis).
Watery Eyes: Red, itchy, and teary eyes (allergic conjunctivitis).
![]() Postnasal Drip: Mucus draining down the back of the throat.
Postnasal Drip: Mucus draining down the back of the throat.
![]() Fatigue: Feeling tired and drained.
Fatigue: Feeling tired and drained.
![]() Headache: A dull ache in the head.
Headache: A dull ache in the head.
![]() Sinus Pressure: A feeling of pressure or pain in the sinuses.
Sinus Pressure: A feeling of pressure or pain in the sinuses.
![]() Cough: May be triggered by postnasal drip or irritated airways.
Cough: May be triggered by postnasal drip or irritated airways.
![]() Dark circles under the eyes (allergic shiners): Caused by congestion of small veins under the eyes.
Dark circles under the eyes (allergic shiners): Caused by congestion of small veins under the eyes.
Causes and Triggers:
![]() Pollen: The most common trigger, especially from:
Pollen: The most common trigger, especially from:![]()

![]() Trees: Spring
Trees: Spring![]()

![]() Grasses: Late spring and summer
Grasses: Late spring and summer![]()

![]() Weeds (especially ragweed): Late summer and fall
Weeds (especially ragweed): Late summer and fall
![]() Mold spores: Can be both indoor and outdoor.
Mold spores: Can be both indoor and outdoor.
![]() Dust mites: Tiny creatures found in dust.
Dust mites: Tiny creatures found in dust.
![]() Pet dander: Dead skin cells shed by animals.
Pet dander: Dead skin cells shed by animals.
![]() Other Irritants: Smoke, strong odors, air pollution can worsen symptoms.
Other Irritants: Smoke, strong odors, air pollution can worsen symptoms.
Diagnosis:
![]() Medical History and Physical Exam: Your doctor will ask about your symptoms, when they occur, and potential triggers.
Medical History and Physical Exam: Your doctor will ask about your symptoms, when they occur, and potential triggers.
![]() Allergy Testing: Helps identify specific allergens that trigger your symptoms. This can be done through:
Allergy Testing: Helps identify specific allergens that trigger your symptoms. This can be done through:![]()

![]() Skin prick test: A small amount of allergen is pricked into the skin.
Skin prick test: A small amount of allergen is pricked into the skin.![]()

![]() Blood test (RAST or ImmunoCAP): Measures the levels of IgE antibodies to specific allergens in your blood.
Blood test (RAST or ImmunoCAP): Measures the levels of IgE antibodies to specific allergens in your blood.
Treatment:
The goal of treatment is to relieve symptoms and improve quality of life. Treatment options include:
![]() Avoidance: The best approach is to avoid the allergens that trigger your symptoms as much as possible. This may involve:
Avoidance: The best approach is to avoid the allergens that trigger your symptoms as much as possible. This may involve:![]()

![]() Staying indoors when pollen counts are high.
Staying indoors when pollen counts are high.![]()

![]() Keeping windows and doors closed.
Keeping windows and doors closed.![]()

![]() Using air conditioning with HEPA filters.
Using air conditioning with HEPA filters.![]()

![]() Washing bedding frequently.
Washing bedding frequently.![]()

![]() Bathing pets regularly.
Bathing pets regularly.![]()

![]() Using dust mite covers on mattresses and pillows.
Using dust mite covers on mattresses and pillows.
![]() Medications:
Medications:![]()

![]() Antihistamines: Block the effects of histamine, reducing itching, sneezing, and runny nose. Available over-the-counter (OTC) and by prescription. Examples include:
Antihistamines: Block the effects of histamine, reducing itching, sneezing, and runny nose. Available over-the-counter (OTC) and by prescription. Examples include:![]()

![]() Older antihistamines (sedating): diphenhydramine (Benadryl), chlorpheniramine (Chlor-Trimeton)
Older antihistamines (sedating): diphenhydramine (Benadryl), chlorpheniramine (Chlor-Trimeton)![]()

![]() Newer antihistamines (non-sedating or less sedating): loratadine (Claritin), cetirizine (Zyrtec), fexofenadine (Allegra)
Newer antihistamines (non-sedating or less sedating): loratadine (Claritin), cetirizine (Zyrtec), fexofenadine (Allegra)![]()

![]() Decongestants: Help to relieve nasal congestion by narrowing blood vessels in the nose. Available as nasal sprays or oral medications. Use with caution and for short periods, as prolonged use can lead to rebound congestion. Examples include:
Decongestants: Help to relieve nasal congestion by narrowing blood vessels in the nose. Available as nasal sprays or oral medications. Use with caution and for short periods, as prolonged use can lead to rebound congestion. Examples include:![]()

![]() pseudoephedrine (Sudafed)
pseudoephedrine (Sudafed)![]()

![]() oxymetazoline (Afrin nasal spray)
oxymetazoline (Afrin nasal spray)![]()

![]() Nasal Corticosteroids: Reduce inflammation in the nasal passages. Generally considered the most effective treatment for allergic rhinitis. Available by prescription and some OTC. Examples include:
Nasal Corticosteroids: Reduce inflammation in the nasal passages. Generally considered the most effective treatment for allergic rhinitis. Available by prescription and some OTC. Examples include:![]()

![]() fluticasone propionate (Flonase)
fluticasone propionate (Flonase)![]()

![]() budesonide (Rhinocort)
budesonide (Rhinocort)![]()

![]() mometasone furoate (Nasonex)
mometasone furoate (Nasonex)![]()

![]() Cromolyn Sodium (NasalCrom): A mast cell stabilizer that helps prevent the release of histamine. Available OTC.
Cromolyn Sodium (NasalCrom): A mast cell stabilizer that helps prevent the release of histamine. Available OTC.![]()

![]() Leukotriene Receptor Antagonists: Block the action of leukotrienes, which contribute to inflammation. Montelukast (Singulair) is a prescription medication in this class.
Leukotriene Receptor Antagonists: Block the action of leukotrienes, which contribute to inflammation. Montelukast (Singulair) is a prescription medication in this class.
![]() Allergy Immunotherapy (Allergy Shots or Sublingual Immunotherapy): Involves gradually exposing you to increasing doses of the allergen to help your body build tolerance. This is a longer-term treatment option and is usually considered for people with severe allergies that are not well-controlled with medications.
Allergy Immunotherapy (Allergy Shots or Sublingual Immunotherapy): Involves gradually exposing you to increasing doses of the allergen to help your body build tolerance. This is a longer-term treatment option and is usually considered for people with severe allergies that are not well-controlled with medications.![]()

![]() Allergy shots (subcutaneous immunotherapy - SCIT): Injections given by an allergist.
Allergy shots (subcutaneous immunotherapy - SCIT): Injections given by an allergist.![]()

![]() Sublingual immunotherapy (SLIT): Tablets dissolved under the tongue.
Sublingual immunotherapy (SLIT): Tablets dissolved under the tongue.
Complications:
While not typically dangerous, hay fever can lead to complications, including:
![]() Sinusitis: Inflammation of the sinuses.
Sinusitis: Inflammation of the sinuses.
![]() Ear infections: Especially in children.
Ear infections: Especially in children.
![]() Sleep disturbances: Due to congestion and other symptoms.
Sleep disturbances: Due to congestion and other symptoms.
![]() Worsening of asthma: Allergic rhinitis can trigger asthma symptoms.
Worsening of asthma: Allergic rhinitis can trigger asthma symptoms.
![]() Decreased quality of life: Symptoms can interfere with daily activities, work, and school.
Decreased quality of life: Symptoms can interfere with daily activities, work, and school.
When to See a Doctor:
![]() If your symptoms are severe and interfere with your daily life.
If your symptoms are severe and interfere with your daily life.
![]() If over-the-counter medications are not providing relief.
If over-the-counter medications are not providing relief.
![]() If you have other health conditions, such as asthma or sinusitis.
If you have other health conditions, such as asthma or sinusitis.
![]() To confirm diagnosis and identify specific triggers.
To confirm diagnosis and identify specific triggers.
In summary, hay fever (allergic rhinitis) is a common allergic condition that causes inflammation of the nasal passages, leading to symptoms like sneezing, runny nose, congestion, and itchy eyes. It's triggered by allergens like pollen, dust mites, pet dander, and mold. Treatment involves avoidance of triggers, medications, and, in some cases, allergy immunotherapy.