Iron Deficiency Anemia
Published: 18 Jun 2025
ICD9: 280.9 ICD10: D50.0 ICD11: 3A00
Iron deficiency anemia is a common type of anemia that occurs when the body doesn't have enough iron.
Iron is a crucial component of hemoglobin, a protein in red blood cells that carries oxygen from your lungs to the rest of your body. When you don't have enough iron, your body can't produce enough hemoglobin, leading to a decrease in red blood cells and therefore, less oxygen circulating throughout your body.
Here's a breakdown of the key aspects:
What it is:
![]() Anemia: A condition in which you don't have enough healthy red blood cells to carry adequate oxygen to your body's tissues.
Anemia: A condition in which you don't have enough healthy red blood cells to carry adequate oxygen to your body's tissues.
![]() Iron Deficiency: The root cause of this specific type of anemia is a lack of iron in the body.
Iron Deficiency: The root cause of this specific type of anemia is a lack of iron in the body.
Causes:
![]() Inadequate Iron Intake: Not consuming enough iron-rich foods in your diet. This is especially common in vegetarians, vegans, and young children.
Inadequate Iron Intake: Not consuming enough iron-rich foods in your diet. This is especially common in vegetarians, vegans, and young children.
![]() Poor Iron Absorption: Certain conditions or medications can interfere with the body's ability to absorb iron from food. These include:
Poor Iron Absorption: Certain conditions or medications can interfere with the body's ability to absorb iron from food. These include:![]()

![]() Celiac disease
Celiac disease![]()

![]() Crohn's disease
Crohn's disease![]()

![]() Gastric bypass surgery
Gastric bypass surgery![]()

![]() Use of certain medications like antacids
Use of certain medications like antacids
![]() Blood Loss: Losing blood faster than your body can replace it. This can be due to:
Blood Loss: Losing blood faster than your body can replace it. This can be due to:![]()

![]() Heavy menstrual periods (menorrhagia)
Heavy menstrual periods (menorrhagia)![]()

![]() Gastrointestinal bleeding (from ulcers, polyps, or cancer)
Gastrointestinal bleeding (from ulcers, polyps, or cancer)![]()

![]() Frequent blood donations
Frequent blood donations![]()

![]() Injury
Injury
![]() Pregnancy: During pregnancy, the body needs more iron to support the growth of the baby. If iron stores aren't sufficient, iron deficiency anemia can develop.
Pregnancy: During pregnancy, the body needs more iron to support the growth of the baby. If iron stores aren't sufficient, iron deficiency anemia can develop.
![]() Growth Spurts: Infants and children, due to their rapid growth, have higher iron requirements.
Growth Spurts: Infants and children, due to their rapid growth, have higher iron requirements.
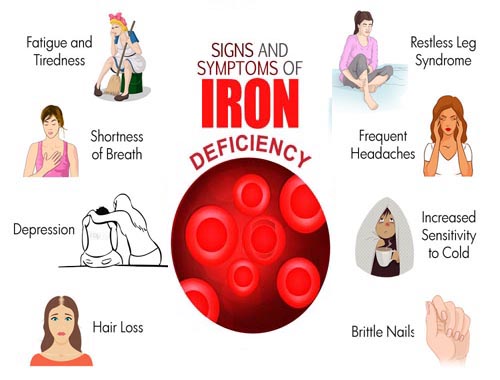
Symptoms:
![]() Fatigue: Persistent tiredness and weakness are the most common symptoms.
Fatigue: Persistent tiredness and weakness are the most common symptoms.
![]() Pale skin: Especially noticeable in the face, nail beds, and inner eyelids.
Pale skin: Especially noticeable in the face, nail beds, and inner eyelids.
![]() Shortness of breath: Even with mild exertion.
Shortness of breath: Even with mild exertion.
![]() Dizziness or lightheadedness: Often due to low blood pressure.
Dizziness or lightheadedness: Often due to low blood pressure.
![]() Headaches: Frequent or persistent headaches.
Headaches: Frequent or persistent headaches.
![]() Cold hands and feet: Due to poor circulation.
Cold hands and feet: Due to poor circulation.
![]() Brittle nails: Nails that chip or break easily.
Brittle nails: Nails that chip or break easily.
![]() Pica: An unusual craving for non-food items like ice, dirt, or clay.
Pica: An unusual craving for non-food items like ice, dirt, or clay.
![]() Restless legs syndrome: An irresistible urge to move the legs, especially at night.
Restless legs syndrome: An irresistible urge to move the legs, especially at night.
![]() Poor appetite, especially in infants and children.
Poor appetite, especially in infants and children.
![]() Difficulty concentrating
Difficulty concentrating
Diagnosis:
![]() Physical Exam: A doctor will check for signs of anemia, such as pale skin and rapid heartbeat.
Physical Exam: A doctor will check for signs of anemia, such as pale skin and rapid heartbeat.
![]() Blood Tests:
Blood Tests:![]()

![]() Complete Blood Count (CBC): Measures red blood cell count, hemoglobin levels, and hematocrit (percentage of blood volume made up of red blood cells). Low hemoglobin and hematocrit are key indicators.
Complete Blood Count (CBC): Measures red blood cell count, hemoglobin levels, and hematocrit (percentage of blood volume made up of red blood cells). Low hemoglobin and hematocrit are key indicators.![]()

![]() Iron Studies: Measures iron levels in the blood, including serum iron, ferritin (iron storage protein), transferrin saturation, and total iron-binding capacity (TIBC). Ferritin is often the most important initial test, as low ferritin levels indicate depleted iron stores.
Iron Studies: Measures iron levels in the blood, including serum iron, ferritin (iron storage protein), transferrin saturation, and total iron-binding capacity (TIBC). Ferritin is often the most important initial test, as low ferritin levels indicate depleted iron stores.
Treatment:
![]() Iron Supplements: Usually prescribed in the form of ferrous sulfate or ferrous gluconate. They should be taken as directed by a doctor, often with vitamin C to improve absorption.
Iron Supplements: Usually prescribed in the form of ferrous sulfate or ferrous gluconate. They should be taken as directed by a doctor, often with vitamin C to improve absorption.
![]() Dietary Changes: Eating more iron-rich foods, such as:
Dietary Changes: Eating more iron-rich foods, such as:![]()

![]() Red meat
Red meat![]()

![]() Poultry
Poultry![]()

![]() Fish
Fish![]()

![]() Beans and lentils
Beans and lentils![]()

![]() Dark green leafy vegetables (spinach, kale)
Dark green leafy vegetables (spinach, kale)![]()

![]() Fortified cereals
Fortified cereals
![]() Treating Underlying Cause: If the anemia is caused by blood loss or poor absorption, the underlying condition needs to be addressed. This might involve medication for ulcers, surgery for polyps, or dietary changes for celiac disease.
Treating Underlying Cause: If the anemia is caused by blood loss or poor absorption, the underlying condition needs to be addressed. This might involve medication for ulcers, surgery for polyps, or dietary changes for celiac disease.
![]() Iron Infusions: In severe cases, or when oral iron is not well-tolerated, iron can be administered intravenously (through a vein).
Iron Infusions: In severe cases, or when oral iron is not well-tolerated, iron can be administered intravenously (through a vein).
![]() Blood Transfusions: In very rare and severe cases, a blood transfusion may be necessary to quickly increase red blood cell levels.
Blood Transfusions: In very rare and severe cases, a blood transfusion may be necessary to quickly increase red blood cell levels.
Prevention:
![]() Eat an Iron-Rich Diet: Consume plenty of iron-rich foods.
Eat an Iron-Rich Diet: Consume plenty of iron-rich foods.
![]() Include Vitamin C: Vitamin C helps the body absorb iron, so eat foods rich in vitamin C (citrus fruits, strawberries, peppers) along with iron-rich foods.
Include Vitamin C: Vitamin C helps the body absorb iron, so eat foods rich in vitamin C (citrus fruits, strawberries, peppers) along with iron-rich foods.
![]() Avoid Iron-Blocking Foods: Limit consumption of foods that can interfere with iron absorption, such as coffee, tea, and calcium-rich foods, when taken with iron supplements or iron-rich meals.
Avoid Iron-Blocking Foods: Limit consumption of foods that can interfere with iron absorption, such as coffee, tea, and calcium-rich foods, when taken with iron supplements or iron-rich meals.
![]() Routine Screening: Pregnant women and individuals at risk for iron deficiency should be screened for anemia regularly.
Routine Screening: Pregnant women and individuals at risk for iron deficiency should be screened for anemia regularly.
Important Considerations:
![]() Don't self-treat: Always consult a doctor before taking iron supplements. Too much iron can be harmful.
Don't self-treat: Always consult a doctor before taking iron supplements. Too much iron can be harmful.
![]() Iron supplements can have side effects: Common side effects include constipation, nausea, and stomach upset. Talk to your doctor about ways to manage these side effects.
Iron supplements can have side effects: Common side effects include constipation, nausea, and stomach upset. Talk to your doctor about ways to manage these side effects.
![]() It takes time to replenish iron stores: It can take several months of iron supplementation to correct iron deficiency anemia.
It takes time to replenish iron stores: It can take several months of iron supplementation to correct iron deficiency anemia.
![]() Follow-up is crucial: Regular blood tests are needed to monitor iron levels and ensure treatment is effective.
Follow-up is crucial: Regular blood tests are needed to monitor iron levels and ensure treatment is effective.
In summary, iron deficiency anemia is a manageable condition. Early diagnosis and treatment are key to preventing complications and improving quality of life. If you suspect you might have iron deficiency anemia, consult your doctor for proper diagnosis and treatment.