Urinary Tract Infection
Published: 18 Jun 2025
ICD9: 599.0 ICD10: N39.0 ICD11: GC08
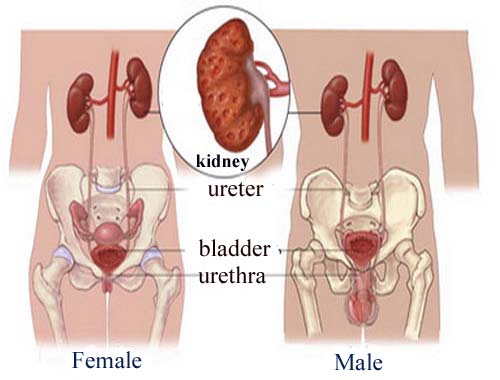
A Urinary Tract Infection (UTI) is an infection in any part of the urinary system, which includes the kidneys, ureters, bladder, and urethra.
Most infections involve the lower urinary tract — the bladder and urethra.
Here's a breakdown:
What causes UTIs?
![]() Bacteria: Most UTIs are caused by bacteria, most commonly *Escherichia coli* (E. coli), which is found in the digestive tract. Other bacteria can also be responsible.
Bacteria: Most UTIs are caused by bacteria, most commonly *Escherichia coli* (E. coli), which is found in the digestive tract. Other bacteria can also be responsible.
![]() How bacteria enter: Bacteria enter the urinary tract through the urethra and begin to multiply in the bladder. The body's natural defenses can usually keep bacteria at bay. However, sometimes these defenses fail, and bacteria can take hold and grow into a full-blown infection.
How bacteria enter: Bacteria enter the urinary tract through the urethra and begin to multiply in the bladder. The body's natural defenses can usually keep bacteria at bay. However, sometimes these defenses fail, and bacteria can take hold and grow into a full-blown infection.
![]() Fungi and Viruses: Less commonly, UTIs can be caused by fungi or viruses.
Fungi and Viruses: Less commonly, UTIs can be caused by fungi or viruses.
Types of UTIs (based on location):
![]() Cystitis (Bladder Infection): This is the most common type of UTI. Symptoms usually include pelvic pressure, lower abdominal discomfort, frequent, painful urination, and blood in the urine.
Cystitis (Bladder Infection): This is the most common type of UTI. Symptoms usually include pelvic pressure, lower abdominal discomfort, frequent, painful urination, and blood in the urine.
![]() Urethritis (Urethra Infection): This involves inflammation of the urethra. Symptoms can include burning with urination and discharge.
Urethritis (Urethra Infection): This involves inflammation of the urethra. Symptoms can include burning with urination and discharge.
![]() Pyelonephritis (Kidney Infection): This is a more serious infection that involves one or both kidneys. Symptoms can include upper back and side (flank) pain, high fever, shaking chills, nausea, and vomiting. Pyelonephritis can lead to permanent kidney damage if left untreated.
Pyelonephritis (Kidney Infection): This is a more serious infection that involves one or both kidneys. Symptoms can include upper back and side (flank) pain, high fever, shaking chills, nausea, and vomiting. Pyelonephritis can lead to permanent kidney damage if left untreated.
Symptoms of UTIs:
![]() Frequent urge to urinate
Frequent urge to urinate
![]() Burning sensation during urination
Burning sensation during urination
![]() Passing frequent, small amounts of urine
Passing frequent, small amounts of urine
![]() Cloudy urine
Cloudy urine
![]() Urine that appears red, bright pink or cola-colored — a sign of blood in the urine
Urine that appears red, bright pink or cola-colored — a sign of blood in the urine
![]() Strong-smelling urine
Strong-smelling urine
![]() Pelvic pain, in women — especially in the center of the pelvis and around the area of the pubic bone
Pelvic pain, in women — especially in the center of the pelvis and around the area of the pubic bone
![]() Rectal pain, in men
Rectal pain, in men
![]() Fever, chills, nausea, and vomiting (especially with kidney infection)
Fever, chills, nausea, and vomiting (especially with kidney infection)
![]() Back pain (especially with kidney infection)
Back pain (especially with kidney infection)
Risk Factors:
![]() Female anatomy: Women have a shorter urethra than men, which means that bacteria have a shorter distance to travel to reach the bladder.
Female anatomy: Women have a shorter urethra than men, which means that bacteria have a shorter distance to travel to reach the bladder.
![]() Sexual activity: Sexual intercourse can introduce bacteria into the urinary tract.
Sexual activity: Sexual intercourse can introduce bacteria into the urinary tract.
![]() Certain types of birth control: Diaphragms and spermicidal agents can increase the risk of UTIs.
Certain types of birth control: Diaphragms and spermicidal agents can increase the risk of UTIs.
![]() Menopause: After menopause, a decline in circulating estrogen causes changes in the urinary tract that make you more vulnerable to infection.
Menopause: After menopause, a decline in circulating estrogen causes changes in the urinary tract that make you more vulnerable to infection.
![]() Urinary tract abnormalities: Babies born with urinary tract abnormalities that don't allow urine to leave the body normally or cause urine to back up in the kidneys are more likely to get UTIs.
Urinary tract abnormalities: Babies born with urinary tract abnormalities that don't allow urine to leave the body normally or cause urine to back up in the kidneys are more likely to get UTIs.
![]() Blockages in the urinary tract: Kidney stones or an enlarged prostate can trap urine in the bladder and increase the risk of infection.
Blockages in the urinary tract: Kidney stones or an enlarged prostate can trap urine in the bladder and increase the risk of infection.
![]() Suppressed immune system: Diabetes, HIV and other conditions that impair your immune system can increase the risk of UTIs.
Suppressed immune system: Diabetes, HIV and other conditions that impair your immune system can increase the risk of UTIs.
![]() Catheter use: People who can't urinate on their own and use a tube (catheter) to urinate have an increased risk of UTIs.
Catheter use: People who can't urinate on their own and use a tube (catheter) to urinate have an increased risk of UTIs.
![]() Recent urinary procedure: Urinary surgery or examination of your urinary tract involving medical instruments can both increase your risk of developing a UTI.
Recent urinary procedure: Urinary surgery or examination of your urinary tract involving medical instruments can both increase your risk of developing a UTI.
Diagnosis:
![]() Urine analysis: A urine sample is examined under a microscope to look for bacteria, white blood cells, and red blood cells.
Urine analysis: A urine sample is examined under a microscope to look for bacteria, white blood cells, and red blood cells.
![]() Urine culture: A urine culture can identify the specific type of bacteria causing the infection and help determine which antibiotics will be most effective.
Urine culture: A urine culture can identify the specific type of bacteria causing the infection and help determine which antibiotics will be most effective.
Treatment:
![]() Antibiotics: Antibiotics are the primary treatment for bacterial UTIs. The specific antibiotic and duration of treatment depend on the type of bacteria causing the infection and the severity of the infection.
Antibiotics: Antibiotics are the primary treatment for bacterial UTIs. The specific antibiotic and duration of treatment depend on the type of bacteria causing the infection and the severity of the infection.
![]() Pain relievers: Over-the-counter pain relievers, such as acetaminophen or ibuprofen, can help relieve pain associated with a UTI.
Pain relievers: Over-the-counter pain relievers, such as acetaminophen or ibuprofen, can help relieve pain associated with a UTI.
![]() Drinking plenty of fluids: Drinking plenty of water helps flush bacteria out of the urinary tract.
Drinking plenty of fluids: Drinking plenty of water helps flush bacteria out of the urinary tract.
Prevention:
![]() Drink plenty of fluids, especially water.
Drink plenty of fluids, especially water.
![]() Wipe from front to back after urination and bowel movements.
Wipe from front to back after urination and bowel movements.
![]() Empty your bladder soon after intercourse.
Empty your bladder soon after intercourse.
![]() Avoid potentially irritating feminine products. (e.g., douches, powders, and sprays)
Avoid potentially irritating feminine products. (e.g., douches, powders, and sprays)
![]() Consider cranberry products (juice or supplements). The evidence is mixed, but some studies suggest they may help prevent recurrent UTIs in some women.
Consider cranberry products (juice or supplements). The evidence is mixed, but some studies suggest they may help prevent recurrent UTIs in some women.
![]() In women with recurrent UTIs after menopause, vaginal estrogen therapy may be helpful.
In women with recurrent UTIs after menopause, vaginal estrogen therapy may be helpful.
Important Notes:
![]() Left untreated, UTIs can lead to serious complications, especially kidney infections. Seek medical attention promptly if you suspect you have a UTI.
Left untreated, UTIs can lead to serious complications, especially kidney infections. Seek medical attention promptly if you suspect you have a UTI.
![]() It is crucial to complete the entire course of antibiotics prescribed by your doctor, even if you start feeling better, to ensure that the infection is completely eradicated.
It is crucial to complete the entire course of antibiotics prescribed by your doctor, even if you start feeling better, to ensure that the infection is completely eradicated.
![]() Recurrent UTIs require further investigation to identify underlying causes.
Recurrent UTIs require further investigation to identify underlying causes.
![]() This information is for general knowledge and does not substitute for professional medical advice. Always consult with a healthcare provider for diagnosis and treatment.
This information is for general knowledge and does not substitute for professional medical advice. Always consult with a healthcare provider for diagnosis and treatment.